AI Model Achieves 97.6% Accuracy in Multiple Sclerosis Diagnosis
A breakthrough AI model demonstrates 97.6% accuracy in diagnosing multiple sclerosis, potentially transforming neurological imaging analysis and accelerating patient diagnosis timelines.
The Race for AI-Driven Neurological Diagnosis Heats Up
The competition to automate medical diagnosis just entered a new phase. A newly developed AI model has achieved 97.6% accuracy in diagnosing multiple sclerosis (MS) from imaging data, marking a significant milestone in the intersection of machine learning and neurology. This breakthrough arrives as healthcare systems worldwide grapple with diagnostic bottlenecks and the growing burden of neurological disease detection.
The development underscores a broader trend: AI systems are increasingly capable of matching or exceeding human radiologist performance in specialized medical imaging tasks. For MS diagnosis—a condition affecting nearly 3 million people globally—the implications are substantial.
Technical Performance and Diagnostic Capability
The 97.6% accuracy figure represents performance across multiple diagnostic dimensions:
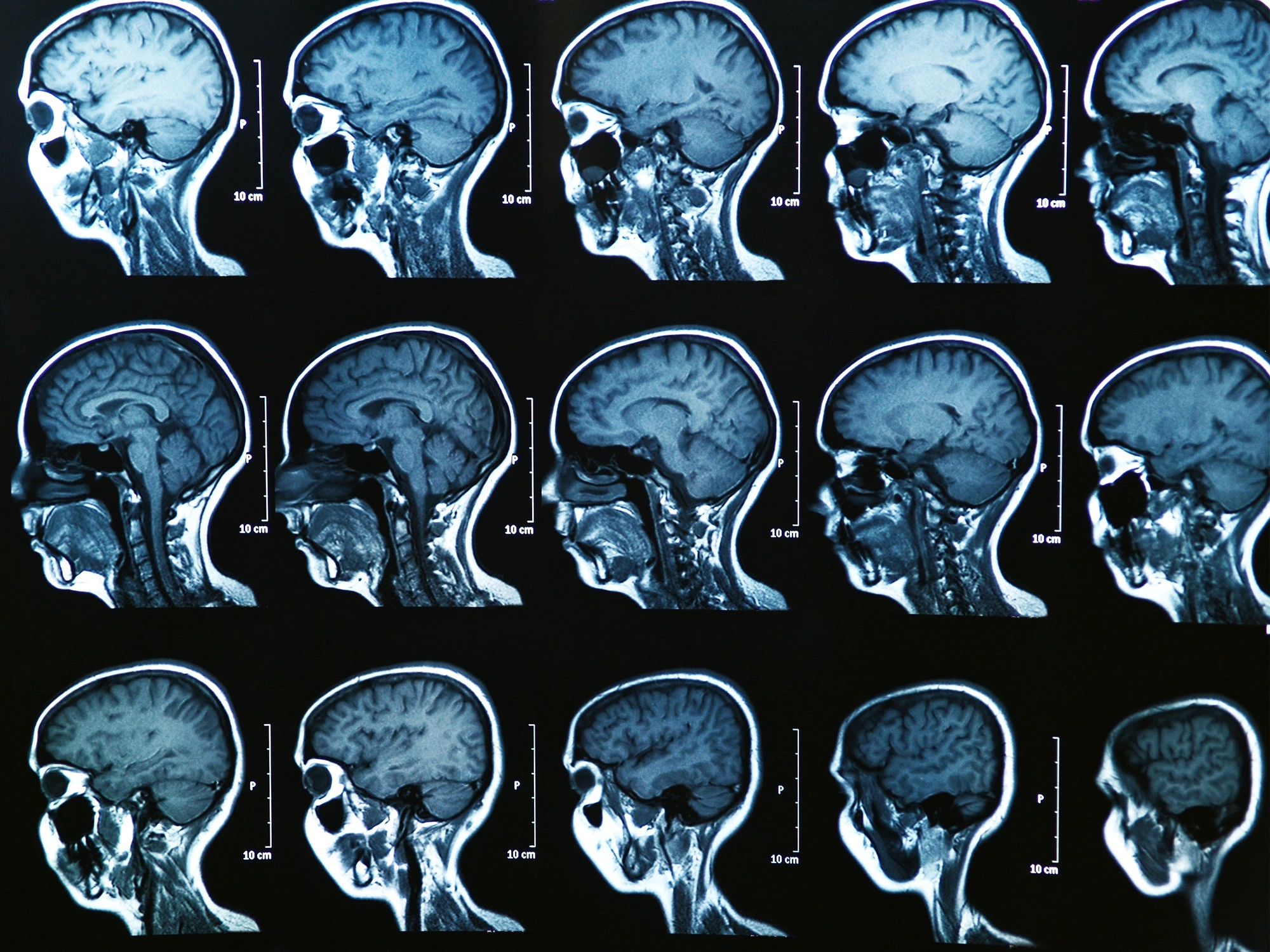
- Detection sensitivity: The model identifies MS lesions in MRI brain scans with high precision
- Subtype classification: Research indicates AI can distinguish between distinct MS subtypes, improving treatment stratification
- Reduced false positives: The model minimizes unnecessary follow-up testing and patient anxiety
The technical architecture likely leverages convolutional neural networks trained on large datasets of annotated MRI scans. This approach has proven effective in other medical imaging domains, where deep learning models can identify subtle patterns invisible to the human eye.
Clinical and Operational Impact
For healthcare providers, the implications extend beyond raw accuracy metrics:
Diagnostic acceleration: MS diagnosis typically requires multiple imaging sessions and specialist review. An AI-assisted workflow could compress this timeline from weeks to days, enabling faster treatment initiation.
Consistency across centers: Healthcare systems implementing AI diagnostic tools report improved standardization in imaging interpretation, reducing variability between institutions.
Resource optimization: Radiologists can redirect time from routine screening to complex cases requiring nuanced clinical judgment, improving overall departmental efficiency.
The Broader Context: AI in Neurology
This achievement doesn't exist in isolation. The medical AI landscape has witnessed accelerating progress:
- Multiple research groups are developing competing MS diagnostic systems
- Regulatory pathways for AI medical devices are maturing, with FDA guidance now established
- Healthcare organizations are increasingly integrating AI tools into clinical workflows
However, the transition from research accuracy to real-world deployment remains challenging. Factors like dataset bias, generalization across different MRI scanner types, and integration with existing hospital IT systems all require careful attention.
Critical Questions Remain
While 97.6% accuracy is impressive, several questions warrant scrutiny:
Validation scope: Was the model tested on independent datasets, or primarily on the training cohort? External validation is essential for credibility.
Clinical context: Does the model account for patient demographics, disease duration, and treatment history—factors that influence MS presentation?
Regulatory status: Has the model undergone FDA review, or is it still in research phase?
The distinction matters significantly. A research-stage model with strong performance metrics differs substantially from a clinically validated, regulatory-approved tool ready for widespread deployment.
Looking Forward
The 97.6% accuracy milestone signals that AI-assisted MS diagnosis is approaching clinical viability. The next phase will involve rigorous prospective studies, regulatory submissions, and careful integration into clinical practice.
For patients with MS, faster and more accurate diagnosis could mean earlier intervention and better long-term outcomes. For healthcare systems, it represents an opportunity to improve diagnostic efficiency while maintaining clinical quality.
The real test, however, lies ahead: whether this laboratory performance translates into tangible benefits when deployed in diverse clinical settings serving real patients.



